QRS complex nomenclature and morphology
Understanding the nomenclature of the QRS complex will help you learn its morphological abnormalities.
Introduction
The QRS complex is one of the waves in an ECG. It is called a complex because it combines more than one wave (usually 2-3 waves).
It comes after the P wave and the PR interval and represents ventricular depolarization.
The different parameters of the QRS complex
When examining a QRS complex, you need to describe your findings in its four different parameters:
Duration - Is the duration normal (i.e. <120 msec)? Is there an interventricular conduction disturbance, like bundle branch blocks or fascicular blocks?
Voltage - Is the voltage normal, i.e. not increased (e.g. in ventricular hypertrophy) or decreased (e.g. in pericardial effusion)?
Axis - What is the QRS axis (normal, left, right or extreme)
Morphology - What do the individual waves of the QRS complex look like?
The QRS nomenclature
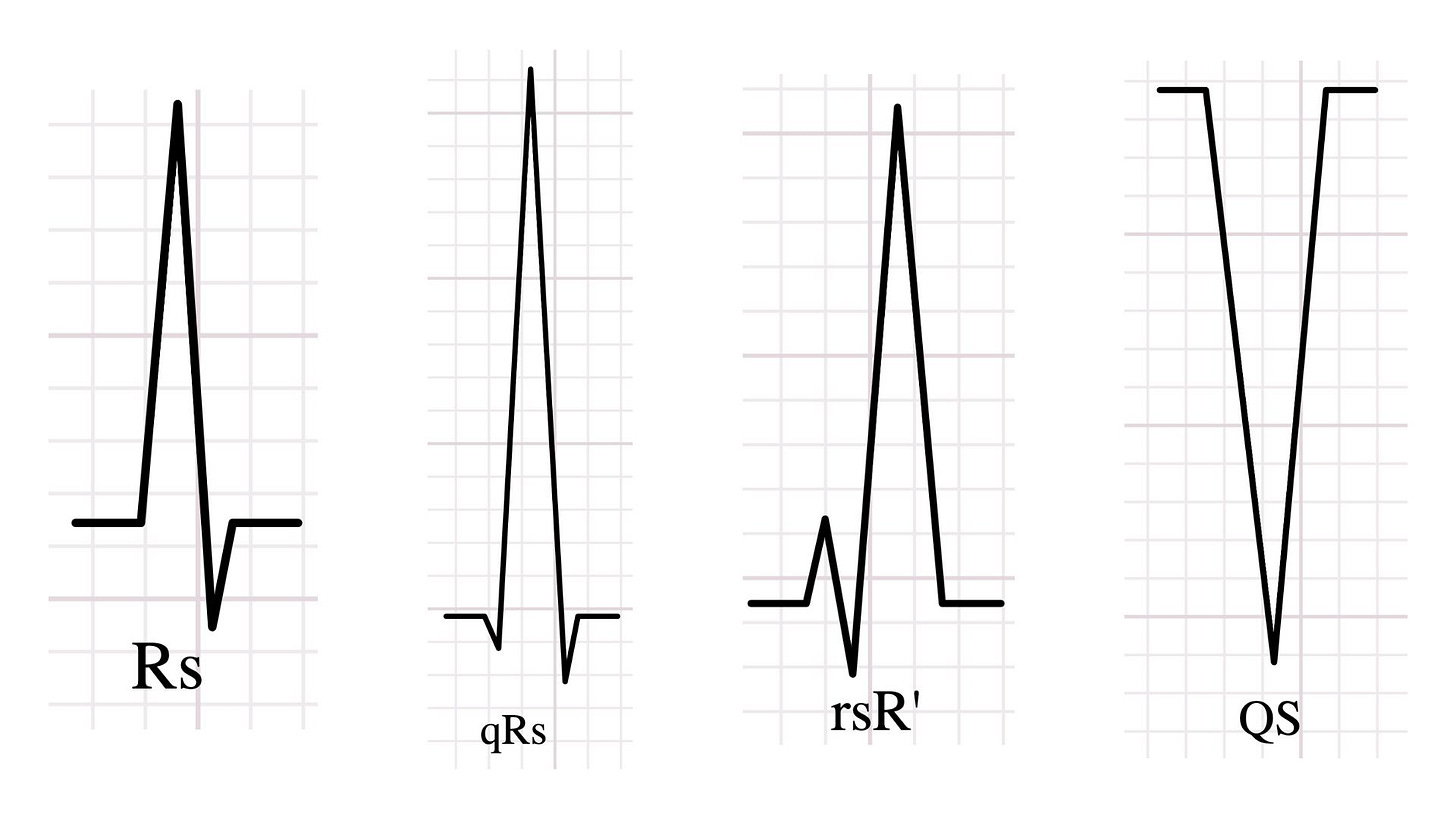
The nomenclature of the QRS complex is essentially the language we use to describe the morphology of the QRS. This is why it’s important to know the following simple rules for naming each wave of the QRS complex:
Q wave = the first negative deflection
R wave = the first positive deflection
S wave = any negative deflection following the R wave
R’ wave = the second positive deflection (if present)
QS wave = an entirely negative QRS complex
Lowercase letters (q, r, or s) describe small amplitude waves of less than 0.5 mV (less than 5 mm with standard calibration) in the QRS complex.
Similarly, uppercase letters (Q, R or S) describe relatively larger amplitude waves of more than 0.5 mV (more than 5 mm with standard calibration) in the QRS complex.
Have a look at some examples to get the gist:
QRS morphology
To explain QRS morphology simply, as ventricular depolarization travels through the ventricles, the mean vector of all activation forces changes direction. This results in the QRS complex comprising 2-3 subsequent deflections with significantly different axes rather than a monophasic positive or negative deflection.
For example, in the following image, we can see why there is typically an rS pattern in V1 and a qR pattern in V6:

Ventricular depolarization starts with the depolarization of the interventricular septum from LEFT to RIGHT, resulting in an initial sum of the electrical vectors (the “resultant” in physics terms) that is directed towards V1, causing a positive deflection in V1, and away from V6, causing a negative deflection in V6.
As the depolarization of the remaining ventricular myocardium occurs, and given that the left ventricular myocardium is larger than the right, the resultant vector faces left, producing a positive deflection in V6 and a negative deflection in V1.
The initial deflection is smaller since the interventricular septum is smaller than the left ventricular myocardium.
Two important abnormalities of the QRS morphology
Having understood the nomenclature of the QRS complex, we can now describe morphological abnormalities. Two important abnormalities are the pathological Q waves and the fragmented QRS.
Pathological Q waves
1) What are pathological Q waves?
A pathological Q wave is a Q wave that is larger than expected, indicating that there has been significant damage to the heart muscle.
ECG criteria for pathological Q waves can be found in the Fourth Universal Definition of Myocardial Infarction (2018). To be honest, these criteria are NOT easy to remember.
For this reason, my approach would be the following:
If I see ANY of the below:
Just the presence of Q waves in V1-V3
Q waves that are more than 1 mm deep in two contiguous leads
I should check the criteria as they are most likely met. You can find the Q wave ECG criteria here (under Table 3).

2) Why do I need to know about pathological Q waves?
Pathological Q waves on an ECG are significant because they can indicate a previous myocardial infarction (MI). This is because the damage to the heart muscle caused by an MI can result in a loss of electrical activity in the affected area, which can lead to the appearance of pathological Q waves.
However, it's important to note that pathological Q waves can also be seen in conditions other than MI, such as myocarditis, cardiomyopathy, and replacement of myocardial tissue by electrically inert tissue, such as amyloid fibrils. Therefore, pathological Q waves should always be interpreted in the context of the patient's clinical presentation.
Fragmented QRS
1) What is a fragmented QRS?
A fragmented QRS (fQRS) is a specific morphological abnormality of the QRS complex. It is characterised by the presence of additional R waves or notches. To put it simply, it's like taking a hammer and smashing the QRS, then putting it back together in a clumsy way because you felt bad about it (joke no 1). Or it’s like 99% of tattoos depicting QRS complexes (joke no 2). I've been told I shouldn't make jokes...

2) Why do I need to know about QRS fragmentation?
The presence of fQRS is more than just an interesting ECG finding. It has been associated with significant cardiac conditions. Studies have shown that fQRS is a predictor of myocardial scar in patients with coronary artery disease. It is also linked to non-ischaemic cardiomyopathy, arrhythmic events in Brugada syndrome, and even pulmonary hypertension and low ejection fraction. Therefore, recognising fQRS can provide valuable insights into a patient's cardiac health and help guide treatment strategies.
3) How is a fragmented QRS created in the first place?
The additional spikes or notches seen in fQRS are thought to be due to the altered sequence of ventricular activation. This alteration can be caused by myocardial scar or fibrosis, which disrupts the normal flow of electrical impulses through the heart. Instead of a smooth wave of electrical activity, the impulses travel around the fibrotic areas (which are electrically inert), shifting the QRS axis temporarily. This leads to the characteristic appearance of fQRS on the ECG.
Summary
The QRS complex represents ventricular depolarization, and it’s a combination of, normally, 2-3 waves.
When examining a QRS complex, you need to describe your findings in its four different parameters:
Duration
Voltage
Axis
Morphology
The nomenclature for naming QRS complex waves includes combining the letters Q, R and S, with uppercase letters representing larger amplitude waves. The nomenclature is the language we use to help us communicate morphological abnormalities of the QRS complex.
Various significant cardiac conditions, especially myocardial infarction and damaged ventricular myocardium, can be indicated by the presence of pathological Q waves and fragmented QRS complexes.
Further reading
Lilly, L. S. (2021). Pathophysiology of Heart Disease (7th ed.). Wolters Kluwer.
Kristian Thygesen and others, Fourth universal definition of myocardial infarction (2018), European Heart Journal, Volume 40, Issue 3, 14 January 2019, Pages 237–269, https://doi.org/10.1093/eurheartj/ehy462
Take Y, Morita H. Fragmented QRS: What Is The Meaning? Indian Pacing Electrophysiol J. 2012 Sep;12(5):213-25. doi: 10.1016/s0972-6292(16)30544-7. Epub 2012 Sep 1. PMID: 23071383; PMCID: PMC3443879.



