Where is the isoelectric line? I asked Reddit…
Should we be using the PR or the TP segment as the isoelectric line?
Some things are better searched for on PubMed instead of Reddit, and this is likely one of them.
HOWEVER… I did get some interesting feedback from fellow ECG enthusiasts, which I think is worth sharing with you.
Why is this important?
Why is it important to identify where the isoelectric line is?
The most obvious answer is to quantify the ST-segment deviation from the baseline, which is crucial when trying to identify the one thing that everyone’s looking for on an ECG: ST elevation in a STEMI.
The PR segment
Is it the PR (or PQ) segment (i.e. from the end of the P wave until the beginning of the Q wave)?
Some researchers argue that ST elevation should be measured from the upper edge of the PR segment and ST depression from the lower edge of the PR segment, therefore supporting the use of the PR segment as the isoelectric line (at least for ST elevation and depression).1
The TP segment
Is it maybe the TP segment (i.e. from the end of the T wave until the beginning of the P wave)?
Other researchers believe that the TP segment is more reliable to be used as a reference point for ST segment deviation, as the PQ segment may change due to atrial lesions.2
The answer Reddit gave me
80 people voted in total
19 voted for the PR-segment
42 voted for the TP-segment
19 voted for both
As you can see from the above, most people supported using the TP segment. Based on some comments, this is most likely due to the well-known specific sign for pericarditis: the widespread PR segment depression (and PR elevation in aVR).
But, interestingly, a significant number of people voted for BOTH. And here is why this is interesting (at least to me…):
THIS is why: PERICARDITIS
Pericarditis can cause a wide range of ECG changes that depend on the timing of the recording. The ECG findings change as the disease resolves.
Pericarditis typically causes widespread PR depression (and PR elevation in aVR), which is a specific but not sensitive sign. This means that while it is a good indicator of pericarditis when present, it is not always present in cases of pericarditis, and its absence does not necessarily rule out pericarditis.
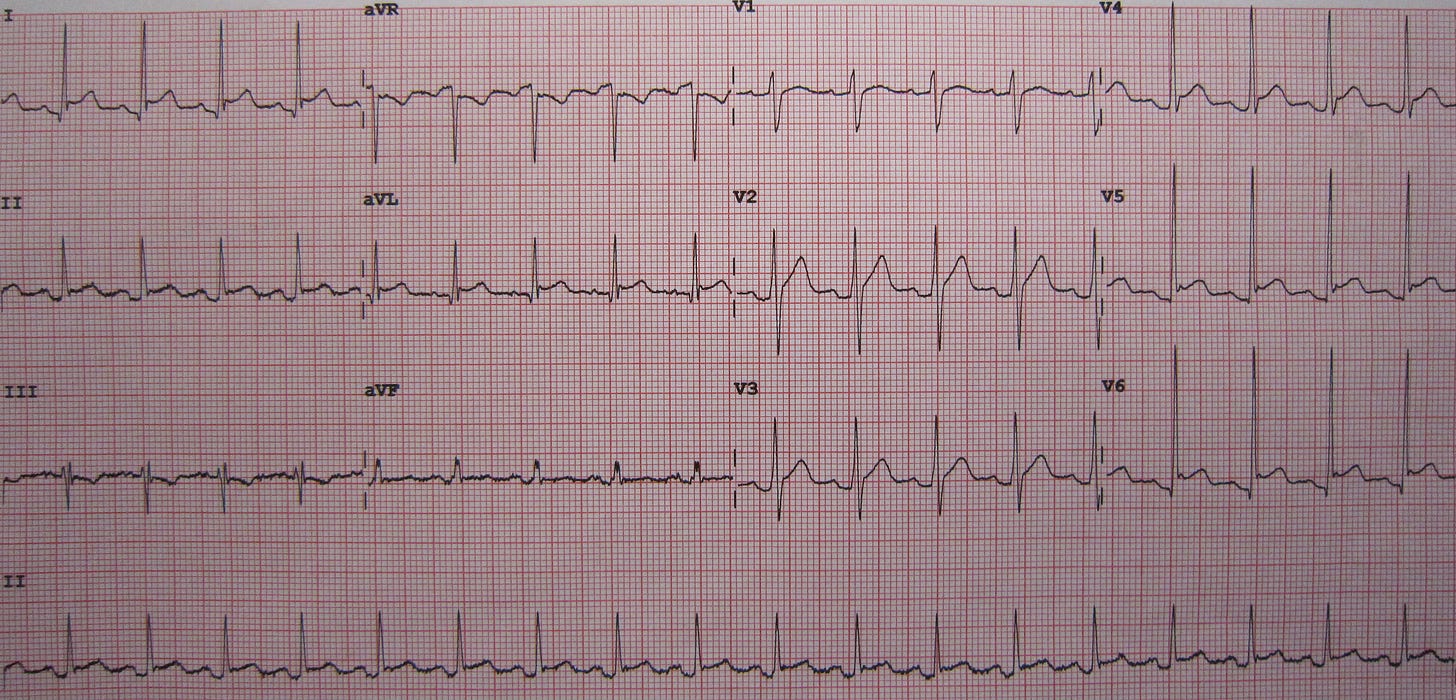
Interestingly, there is a lesser-known sign of pericarditis that affects the TP segment, called Spodick’s sign: downsloping TP elevation (best visualised in lead II).
So… what’s the right answer?
Honestly, I don’t know…
Personally, I most frequently use the TP segment, which seems to be a common practice among most people.
Nevertheless, it is important to be aware of the various reasons why one method may be less accurate than another in certain circumstances.
Smith SW, Whitwam W. Acute coronary syndromes. Emerg Med Clin North Am. 2006 Feb;24(1):53-89, vi. doi: 10.1016/j.emc.2005.08.008. PMID: 16308113.
Coppola G, Carità P, Corrado E, Borrelli A, Rotolo A, Guglielmo M, Nugara C, Ajello L, Santomauro M, Novo S; Italian Study Group of Cardiovascular Emergencies of the Italian Society of Cardiology. ST segment elevations: always a marker of acute myocardial infarction? Indian Heart J. 2013 Jul-Aug;65(4):412-23. doi: 10.1016/j.ihj.2013.06.013. PMID: 23993002; PMCID: PMC3860734.





