Atrial Fibrillation
What is atrial fibrillation (AF) and why all healthcare professionals should know about it?
What is atrial fibrillation (AF)?
In the 2020 ESC guidelines on atrial fibrillation, AF is defined as follows:
“A supraventricular tachyarrhythmia with uncoordinated atrial electrical activation and consequently ineffective atrial contraction.” [2]
Supraventricular: The location of the arrhythmia is in the atria
Tachyarrhythmia: The atrial depolarisation rate is > 100 per minute1
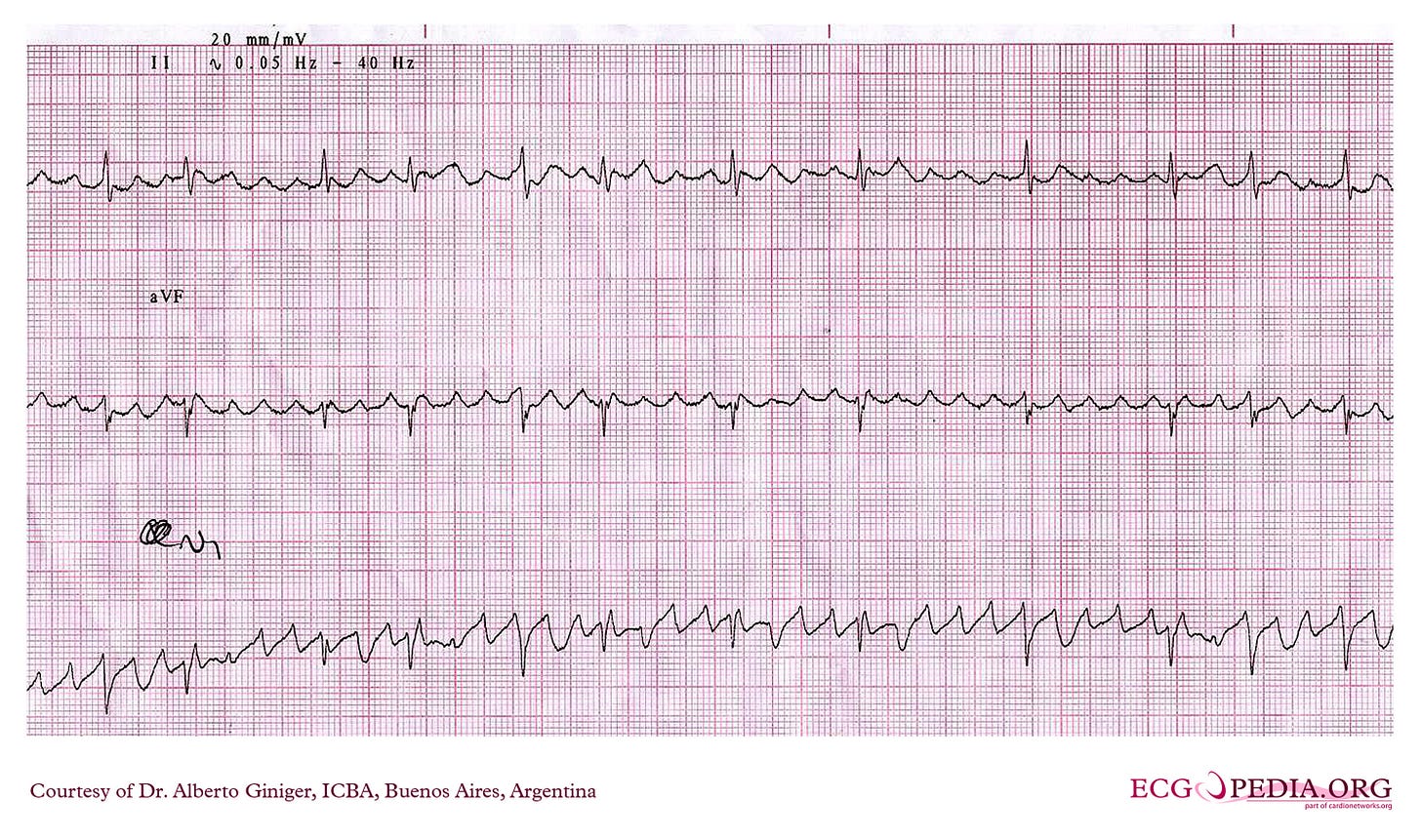
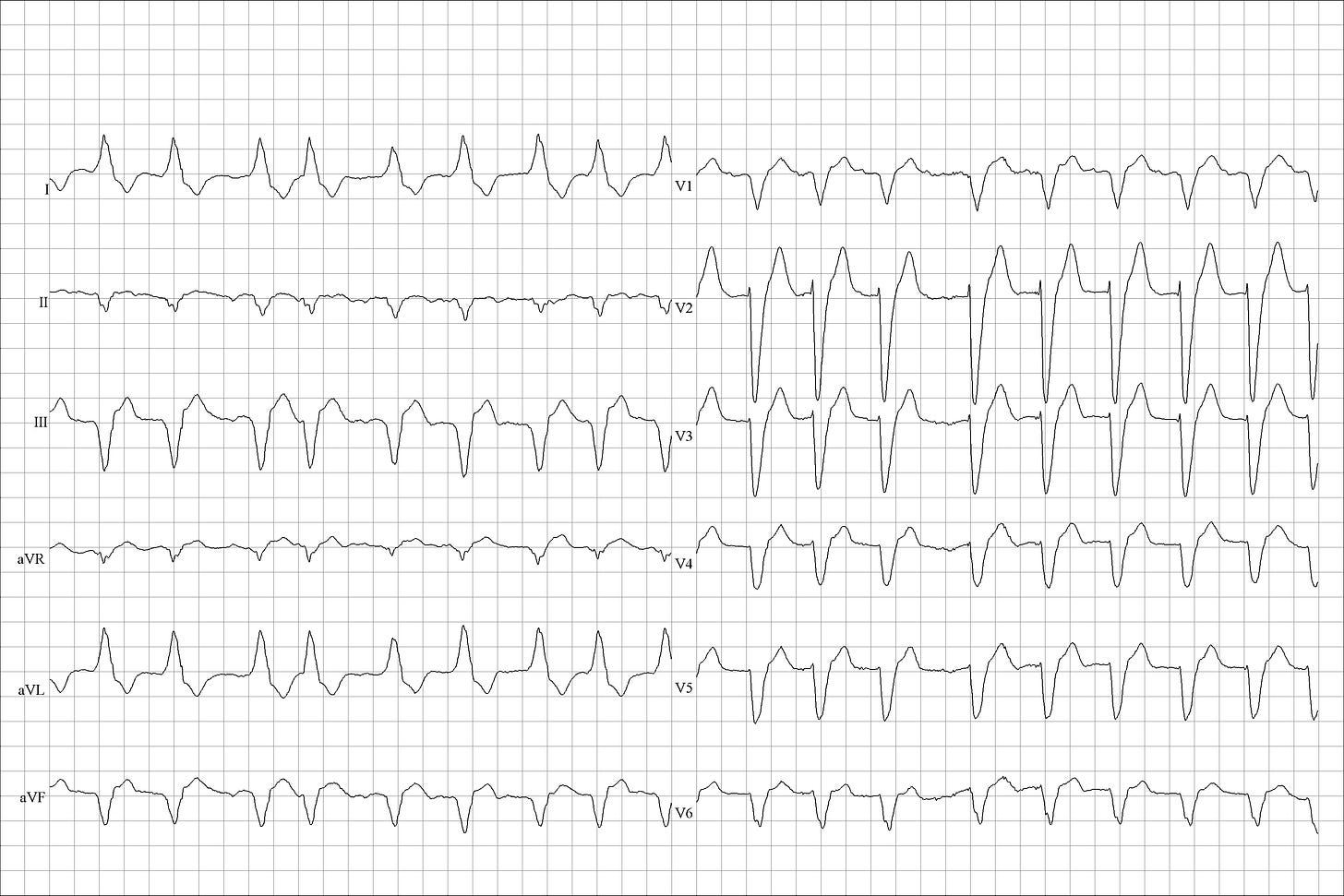
Uncoordinated atrial electrical activation: The atrial electrical activity is normally organised in what we see as the “P wave” on the transthoracic ECG. In AF, the atria fibrillate and the underlying fibrillatory waves present in a spectrum from almost flat to very prominent (mimicking flutter waves) (see images below).
Ineffective atrial contraction: The coordinated depolarisation of the atria will normally lead to a coordinated atrial contraction, known as the “atrial kick”. The atrial kick can be responsible for 20-30% of the blood volume transferred to the ventricles. In AF, you lose the atrial kick. [3]

The “irregularly irregular” pattern
In AF, the atria fibrillate with a rate of 350-600 bpm! [4] Thankfully, we have the AV junction (AV node and His bundle), the heart’s timekeeper, that protects the ventricles from depolarising so fast, which would cause them to fibrillate and produce zero cardiac output!
The AV junction protects the ventricles due to its electrophysiological properties: it has a long refractory period (meaning that once it’s depolarised, it becomes refractory for a long time, during which it cannot be depolarised again). Its red traffic light stays on longer than the traffic lights elsewhere in the heart.
So, the AV junction allows some atrial depolarisations to travel down to the ventricles. And, because the atrial depolarisations are so many, they are allowed down to the ventricles in an irregularly irregular pattern. Please note that both words are important: irregularly irregular. The first (“irregularly”) tells us there’s no way for us to predict when the next wave to come down to the ventricles will be. There is no predictability, no pattern to this irregularity.2
Diagnosing clinical AF
Knowing the above, you can understand the diagnosis of clinical AF:3
“A standard 12-lead ECG recording OR a single-lead ECG tracing of ≥ 30 s showing heart rhythm with no discernible repeating P waves AND irregular RR intervals (when atrioventricular conduction is not impaired) is diagnostic of clinical AF.” [2]
Classifying AF
There are five AF patterns:
First diagnosed
Paroxysmal (terminates within 7 days of onset)
Persistent (continuous beyond 7 days, but less than 12 months)
Long-standing persistent (continuous beyond 12 months)
Permanent (the patient and doctor have accepted the AF and are not planning rhythm control management)
The prevalence of AF
AF is the most commonly treated cardiac arrhythmia. Please note: the most commonly treated cardiac arrhythmia. Sinus tachycardia is very common as well, but we don’t treat it; we treat its underlying causes if needed.
Why is AF the most commonly treated cardiac arrhythmia?
To answer this, we need to take a look at the risk factors for developing AF:
Age: The possibility of developing AF increases with age, and AF is uncommon before the age of 50.
Coronary artery disease (CAD)
Heart failure (HF)
Valvular heart disease
Hypertension
Alcohol intake
Obesity
Sleep-apnoea syndrome
Diabetes mellitus [1]
These are all very common problems clinicians encounter in practice, which is why AF is so common.
And this is just a list of common risk factors for developing AF. Other less common factors, such as hyperthyroidism, cardiac surgery and engaging in endurance athletics, can also cause AF. [1]
The impact of AF
AF has a significant impact on lives and healthcare systems.
Why? Because of the significance of the sequelae of AF, which include the following:
1. Thromboembolism
In AF, the atria don’t contract normally, resulting in blood stasis. This stasis increases the risk of thrombus formation inside the atria, especially in the left atrial appendage.
This thrombus can subsequently move to any part of the arterial system, causing a thromboembolic event which can have massive consequences for the patient:
Stroke
Myocardial infarction (from thromboembolism, not due to coronary artery disease)
Mesenteric ischaemia [5][6]
2. Myocardial infarction
Apart from thromboembolism, an MI can also occur from a supply-demand mismatch, leading to ischaemia.
A rapid heart rate secondary to AF with rapid ventricular response (RVR) increases the oxygen demand of the myocardium. This demand sometimes is not met with the supply, especially in otherwise unhealthy hearts, leading to a Type 2 MI (from demand ischaemia). [5]
3. Heart Failure
The presence of HF or AF increases the possibility of developing the other over time. [7]
4. Mortality
AF is an independent risk factor for mortality in both males and females and across a wide age range. [5]
5. Cognitive impairment and dementia
Atrial fibrillation is linked to a higher risk of developing dementia, even if there is no history of stroke. [8]
Managing AF: A multidisciplinary approach
The main aspects of the AF management are the following: [2]
1. Anticoagulation
Anticoagulation is needed to reduce the risk of thromboembolism (stroke, most notably).
The thromboembolic risk is assessed using the CHA2DS2-VASc score.
The HAS-BLED score is useful to assess the bleeding risk and to help address modifiable bleeding risk factors.
Balancing the thromboembolic and bleeding risk is always a priority when managing AF.
2. Rate control
Rate control is important to prevent the sequelae from a rapid ventricular rate (such as Type 2 MI and Arrhythmia-induced Cardiomyopathy), as well as for symptom control.
3. Rhythm control
Rhythm control is also important for symptom control and for reducing the risk of the aforementioned sequelae.
As mentioned above, this part of the management is not indicated for permanent AF. In permanent AF, by definition, the patient and the doctor have accepted the AF and are not planning to rhythm-control it.
The need for a multidisciplinary approach
The causes, effects and management of AF are spread throughout many different medical specialities and even to other fields of healthcare, such as nutrition.
Adherence to pharmacological treatment is extremely important (for example, with anticoagulation, especially when electrical cardioversion is planned in the future).
Therefore, to manage AF, you need a multidisciplinary approach and proper patient education.
Conclusion
Atrial fibrillation poses a major challenge to patients and healthcare systems.
It’s the most commonly treated cardiac arrhythmia.
It’s a complex problem that requires a holistic and multidisciplinary approach. Key parts of management include anticoagulation, rate control, and rhythm control.
A Lighter Note: The "Fast AF" Anecdote
I came across a funny meme, but I couldn't find it to share. Here's what I remember:
During the cardiology ward round:
If you’re the SHO in this case, the reason the cardiology registrar will try to keep your mouth shut is because there’s only fast AF. AF is a tachyarrhythmia; therefore, it’s always fast. What you meant to say is that the ventricular response is fast. Now that’s technically not the same thing as fast AF.
Another reason why you should avoid saying fast AF is inspired by a real-life story:
A colleague of mine was on a respiratory medicine ward round. They encountered a patient with AF and RVR, awaiting rate control before being discharged. The consultant, explaining the situation, told the patient they were in "fast AF".
After the consultation, the patient chatted with the person in the next bed.
"Are you heading home soon?" the neighbouring patient asked.
"Not just yet, maybe later or tomorrow," our patient responded.
"But I thought they'd discharge you today!"
The patient smirked, "The doc said they need to fix my heart. Apparently, it's going 'fast as f...ck'!"
Thanks for reading
References
Brian Olshansky, Rishi Arora. Mechanisms of atrial fibrillation. Post TW, ed. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2022.
Gerhard Hindricks and others, 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC, European Heart Journal, Volume 42, Issue 5, 1 February 2021, Pages 373–498, https://doi.org/10.1093/eurheartj/ehaa612
Kurapati R, Heaton J, Lowery DR. Atrial Kick. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482421/
Goodacre S, Irons R. ABC of clinical electrocardiography: Atrial arrhythmias. BMJ. 2002 Mar 9;324(7337):594-7. doi: 10.1136/bmj.324.7337.594. Erratum in: BMJ 2002 Apr 27;324(7344):1002. PMID: 11884328; PMCID: PMC1122515.
Kapil Kumar, MD. Atrial fibrillation: Overview and management of new-onset atrial fibrillation. Post TW, ed. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2023.
Aziz AA, Christmas D. Acute Mesenteric Ischemia in a Chronically Anticoagulated Patient With Atrial Fibrillation: Anticoagulation Reversal, Management and Preventing Recurrence. Cureus. 2022 Jan 26;14(1):e21642. doi: 10.7759/cureus.21642. PMID: 35233319; PMCID: PMC8881081.
Brian Olshansky, MD. The management of atrial fibrillation in patients with heart failure. Post TW, ed. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2022.
Eric B Larson, MD, MPH. Risk factors for cognitive decline and dementia. Post TW, ed. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2019.
This doesn't mean that the ventricular depolarisation rate is going to always be fast (AF with rapid ventricular response). The ventricular depolarisation rate could be normal (AF with normal ventricular response) or even slow (AF with slow ventricular response). But the atrial depolarisation rate is, by definition, fast.
Please note that AF produces an irregularly irregular ventricular response when there is no underlying problem in atrioventricular conduction. When you have a 3rd-degree AV block, because no atrial depolarisations get transferred to the ventricles either way, you will most likely have regular RR intervals, even in AF. This regularity is caused by the junctional or ventricular escape rhythm in the 3rd-degree AV block.
There are two other types as well: the atrial high-rate episode and subclinical AF, which are beyond the scope of this post. Find out more in the 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation.





Very interesting read. On the quiz it mentioned PE was unlikely as the clots only tend to form in the left atrium. Is there any reason for this? I’d always assumed it could form in either.