Atrioventricular conduction delay: an overview
A brief summary of the electrocardiographic features of AV blocks.
Introduction
Definition of atrioventricular (AV) conduction delay
Atrioventricular conduction delay refers to a delay in the transmission of an impulse from the atria to the ventricles.1
Assessing for AV conduction delay on a 12-lead transthoracic ECG
Generally, atrioventricular (AV) conduction is evaluated by assessing the relationship between the P waves and QRS complexes.
Specifically, on a 12-lead transthoracic ECG, atrioventricular conduction is assessed in two ways:
The length of the PR interval
Whether the P wave leads to a QRS or not
When either of the two is abnormal, you have an AV block.
Anatomy of AV blocks
So when you do have an AV block, at which part of the conduction system does the problem originate?
Think of it this way: what does the PR interval reflect (remember: the PR interval includes the P wave)?
P wave: atrial depolarization (SA nodal depolarization precedes atrial depolarization)
PR segment: the depolarization of all the elements of the conduction system until electrical signals reach the ventricles (AV node → His bundle → bundle branches → Purkinje fibers)

(Please note that SA nodal depolarisation produces a very small voltage which is non-recordable on a 12-lead transthoracic ECG. It can be seen, however, if you had an intracardial lead placed close to the SA node.)
Naturally, any part of the aforementioned conduction pathway can be responsible for AV blocks.
The PR interval varies with the heart rate
The PR interval is not fixed; it varies with the heart rate (HR). Basically, it can be influenced by the vagal tone, as HR can:
↑ vagal tone (↓ sympathetic tone) → ↓ HR → ↑ PR interval
↓ vagal tone (↑ sympathetic tone) → ↑ HR → ↓ PR interval
Categories of AV blocks
1st degree AV block
2nd degree AV block Mobitz I (Wenckenbach)
2nd degree AV block Mobitz II
3rd degree AV block (complete AV block)
Special categories
2:1 AV block
High grade AV block
Variable AV block
Let’s get started!
1st degree AV block

See the correct answer in the second footnote.2
First-degree AV block is not a true block but rather a delayed or slowed AV conduction, characterised by a prolonged PR interval (>200 ms at resting heart rates). It is more appropriate to use the term “prolonged AV conduction” instead of AV block.
All P waves are conducted, so there is 1:1 AV conduction. It’s just that the PR interval is more than 200 msec.
Is 1st-degree AV block caused by a delay in the AV node? Not necessarily. Electrophysiological studies have shown that PR interval prolongation could be due to conduction delay located at the atrioventricular node, right atrium, or the His-Purkinje system. However, the most commonly affected place is the AV node.
Is it always abnormal? No. For example, as we mentioned above, the PR interval is influenced by the vagal tone. Therefore, in athletes who normally have sinus bradycardia, it would be completely normal for them to have a first-degree AV block when their resting heart rate is, say, 30 bpm.
What you see:
PR interval > 200 ms (over five small squares at 25 mm/s)
Every P wave is still followed by a QRS (1:1 conduction)
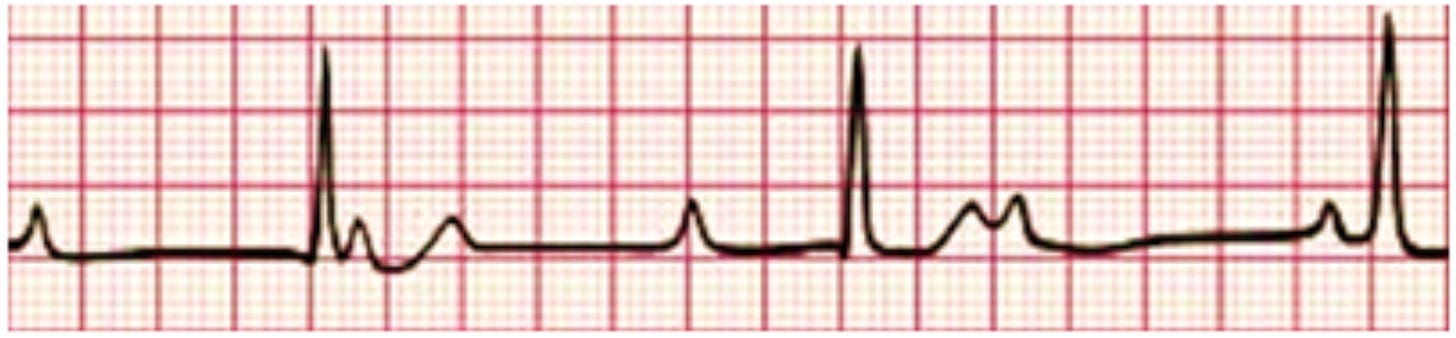
2nd degree AV block Mobitz I (Wenckenbach)

In Mobitz type I (Wenckebach) condition, there’s a progressive prolongation of the PR interval (AV conduction) until an atrial impulse is completely blocked. This results in a P wave without a QRS complex, often referred to as a “dropped beat.”
Mobitz type I occurs because each depolarisation results in the prolongation of the refractory period of the atrioventricular (AV) node (Wenckenbach phenomenon). When an atrial impulse passes through the AV node during the relative refractory period, it conducts more slowly, prolonging the PR interval. Eventually, an impulse arrives when the AV node is in its absolute refractory period and will not be conducted.
What you see:
Gradual prolongation of the PR interval
Eventually a P wave “drops” (no QRS) (intermittent AV conduction)
2nd degree AV block Mobitz II

In Mobitz type II, there’s a constant PR interval across the rhythm strip, both before and after the non-conducted atrial beat. Each P wave is associated with a QRS complex until there’s one atrial conduction or P wave that isn’t followed by a QRS. Mobitz type II is often a problem in the infra-nodal conduction system.
In contrast to Mobitz type I, there’s no change in the PR interval (i.e. the PR interval is normal). This is because the His-Purkinje system is all or none, meaning it either conducts (always at the same rate) or doesn’t conduct an impulse.
Mobitz type II has a higher risk of progression to complete AV block than Mobitz type I and is usually an indication for a pacemaker, even if asymptomatic. If complete heart block were to develop, the escape rhythm is almost always ventricular and wide complex (due to the fact that it’s often a problem in the infra-nodal conduction system).
What you see:
PR interval remains fixed and normal
Sudden non‑conducted P wave (intermittent AV conduction)
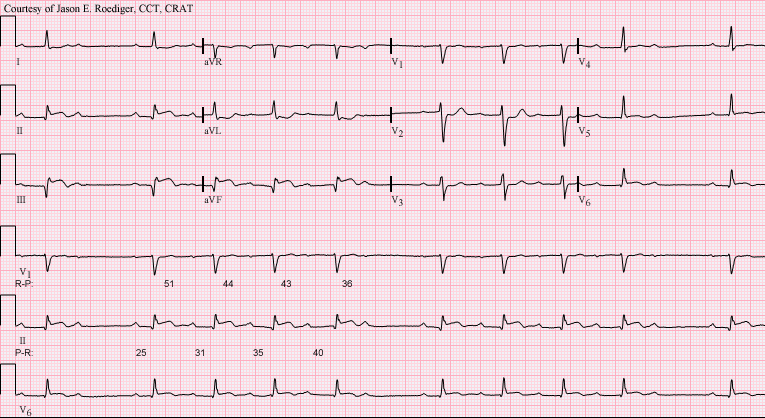
3rd degree AV block (complete AV block)
The 3rd-degree AV block, also known as complete AV block, is characterised by the complete absence of impulses from the atria reaching the ventricles. This results in a complete dissociation between the atria and ventricles (called atrioventricular (AV) dissociation).
While the atria continue to function at a steady rhythm, the ventricles activate through an escape rhythm, which can be mediated by the AV junction (junctional escape), one of the fascicles (fascicular escape), or by the ventricular myocytes themselves (ventricular escape rhythm).
The image above demonstrates a complete AV block with a junctional escape rhythm. This is evident because the QRS complex is not prolonged, indicating that the escape rhythm originates from the AV junction and travels down to the ventricles via the normal pathway.
As a result of this block, the heart rate typically falls below 60 bpm (usually less than 40 bpm if the escape rhythm is ventricular), and most patients experience hemodynamic instability.
What you see:
PR interval is not defined, as there is no association between the atrial and ventricular rhythms (atrioventricular (AV) dissociation)
Independent atrial/ventricular activity: P waves march at their own rate and QRS at a slower escape rhythm
Special categories of AV block
2:1 AV block

As the question suggests, this is a specific type of 2nd-degree AV block.
The correct answer is that we can’t be certain if it’s a Mobitz I or Mobitz II AV block. To determine if it’s Mobitz I or II, you need at least three P waves – the third one being the one that doesn’t conduct to the ventricles. This helps distinguish between progressive PR prolongation (Mobitz I) and non-progressive PR prolongation (Mobitz II).
However, Mobitz I usually starts with a prolonged PR interval, regardless of the type. Given that the PR interval in the ECG above is around 180 ms (which is normal), it makes it more likely to be a Mobitz II AV block.
High grade AV block
A high-grade (or advanced) AV block is when you have ≥2 consecutive, non-conducted P waves.
Imagine something like 2nd-degree AV block Mobitz II, but instead of having only one dropped beat and then the cycle restarting again, you have at least 2 consecutive dropped beats.
See example of high-grade AV block here: https://www.ncbi.nlm.nih.gov/books/NBK459147/figure/article-36720.image.f4/?report=objectonly
Variable AV block
Variable AV block occurs when the conduction ratio is not constant. For instance, it’s not just 3:2 or 4:3, but it can vary. This is commonly seen in atrial flutter or atrial tachycardia, which is why you’d observe an irregular ventricular response in these rhythms.
For example, atrial flutter has an atrial activity rate of around 300 bpm. The AV node typically doesn’t allow such frequent electrical signals to be conducted to the ventricles, protecting them and enabling proper filling and maintaining cardiac output. Consequently, the lowest level of AV block we usually observe in atrial flutter is 2:1, resulting in a ventricular rate of 150 bpm.
However, sometimes, you may see 2:1, followed by a few beats later, it becomes 3:1, then 2:1 again, and possibly even 4:1. This demonstrates a variable degree of AV block within a case of atrial flutter.
This is usually a normal response and doesn’t indicate conduction system disease.
Example
See the correct answer in the third footnote. 3
Summary
These are the basic AV block types at a glance:
Get in touch if you have any questions!
Further reading
Kashou AH, Goyal A, Nguyen T, et al. Atrioventricular Block. [Updated 2024 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459147/
Oldroyd SH, Quintanilla Rodriguez BS, Makaryus AN. First-Degree Heart Block. [Updated 2023 Jan 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448164/
Mangi MA, Jones WM, Mansour MK, et al. Second-Degree Atrioventricular Block. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482359/
Knabben V, Chhabra L, Slane M. Third-Degree Atrioventricular Block. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545199/
Spies F, Knecht S, Zeljkovic I, Reichlin T, Madaffari A, Osswald S, Sticherling C, Kühne M. First-degree atrioventricular block in patients with atrial fibrillation and atrial flutter: the prevalence of intra-atrial conduction delay. J Interv Card Electrophysiol. 2021 Aug;61(2):421-425. doi: 10.1007/s10840-020-00838-3. Epub 2020 Jul 30. PMID: 32734408; PMCID: PMC8324594.
You will also see them being referred to as heart blocks. But this terminology is too vague. In the heart, there are many kinds of blocks: AV blocks, bundle branch blocks, fascicular blocks, sinoatrial blocks… Therefore, the term “heart blocks” is not useful.
The correct answer is 360 ms (the length of the PR interval - from the start of the P wave until the start of the QRS complex is 9 mm, which is 9 x 40 ms = 360 ms, if the recording speed is 25 mm/s).
The correct answer is 2nd degree AV block Mobitz I. You can see that therer’s a progressive prolongation of the PR interval until a P wave is not conducted at all. For every 5 P waves, only 4 are conducted (resulting in 4 QRS complexes). Therefore, the ratio of AV conduction is 5:4.




