Productive cough and chest pain; not what you'd think | ECG challenge #3
Does a productive cough mean infection, or could it potentially be something else?
Clinical case
A 74-year-old man has chest pain and is brought to the emergency department. He also reports a 2-day history of fever and cough with 'dark brown' sputum.
His blood pressure is 100/60 mmHg, pulse is 100 bpm, and respiratory rate is 28 breaths/min. Oxygen saturation is 89% on room air.
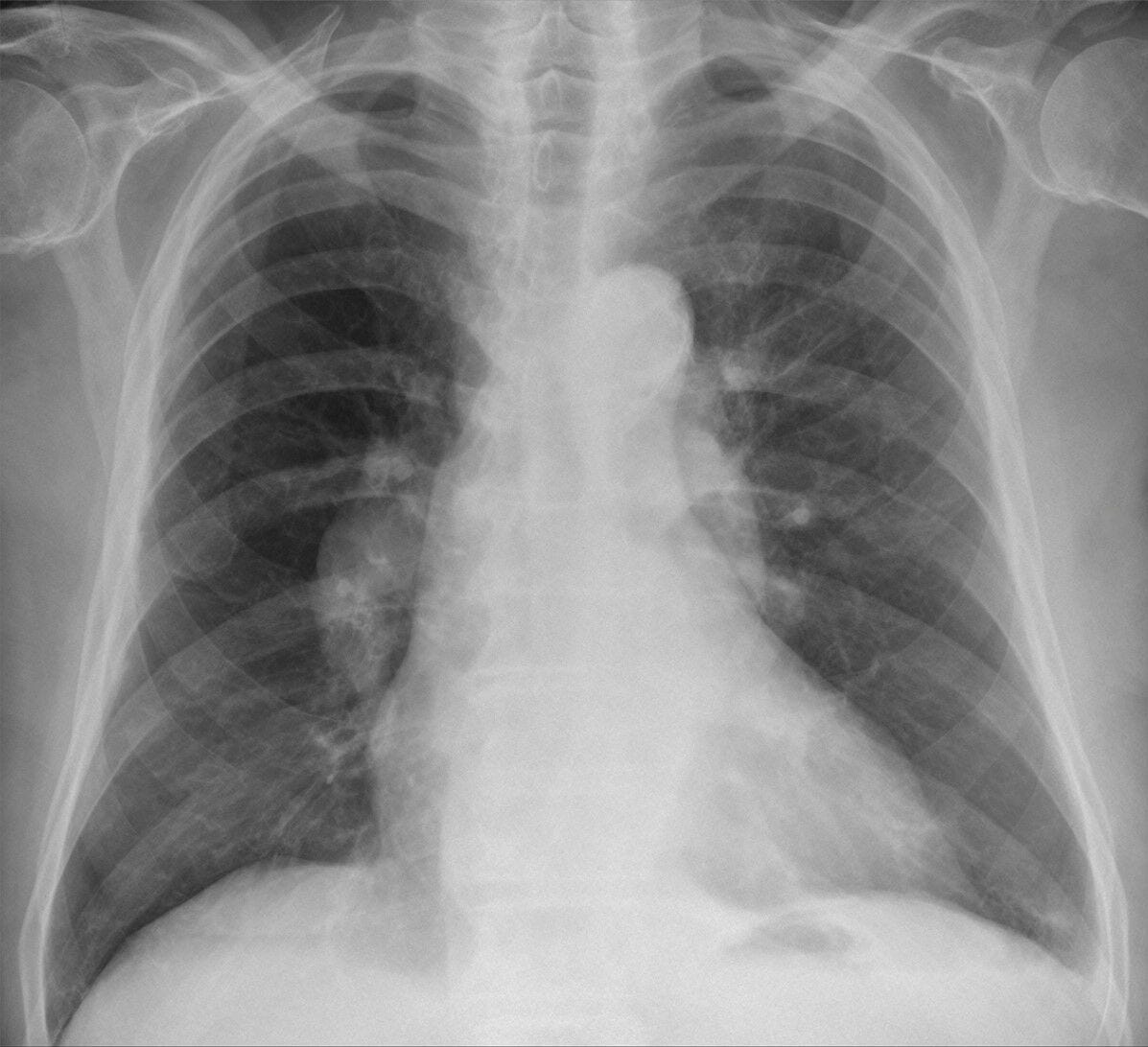
An image of a PA chest X-ray is provided below.
This scenario is based on a real case.
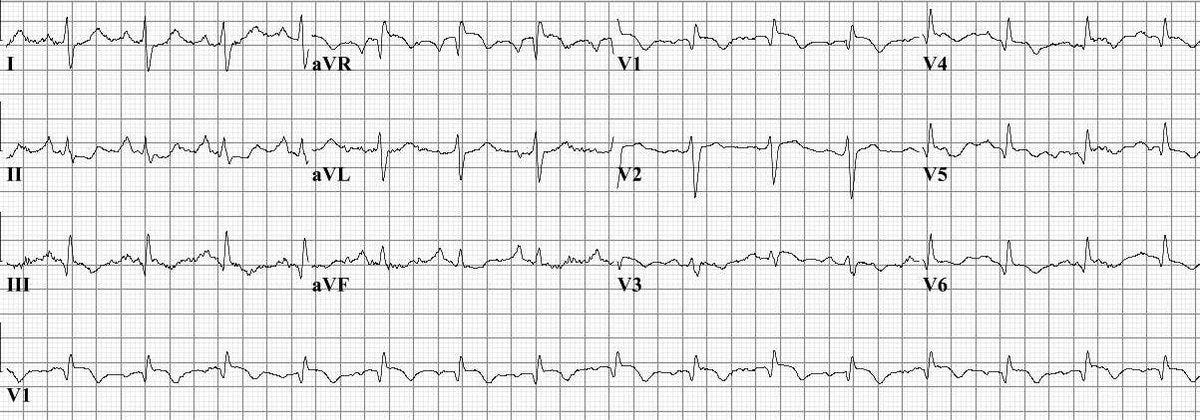
ECG systematic analysis
Although the paper recording speed and voltage calibration are not reported, we’ll assume it to be 25 mm/s, and 10 mm/mV, respectively (standard).
This ECG shows the following:
Rhythm: Sinus tachycardia
P waves: Normal axis and rate is 100 bpm. The morphology is abnormal
P pulmonale (> 2.5 mm tall in leads II, III, aVF)
PR interval: 180 ms (normal) and 1:1 AV conduction
QRS complex:
Duration: Slightly prolonged but not abnormal (around 110 msec).
Axis: Borderline right axis (notice how lead I is neither positive nor negative, and lead aVF is positive - so the axis must be around +90 degrees).
Morphology: Q wave in leads III, V4-V6 and deep S wave in lead I (therefore S1Q3T3 sign positive). qR pattern in V1 but no RS in lead V6.
Voltage: Normal
QT interval: 465 ms (QTcB)
ST Segment: ST depression in leadd II and aVF
T waves: Inverted T waves in leads III, V3-V6 and flat T waves in lead aVF
Overall: sinus tachycardia, P pulmonale, S1Q3T3, repolarisation abnormalities inferolaterally.
Correct answer
The correct answer is sinus tachycardia.
This patient presents with acute onset chest pain, hypoxaemia, tachycardia, and haemodynamic instability, all of which are classic features of acute pulmonary embolism (PE).
Fever can manifest in thrombotic states. Additionally, the productive cough with 'dark brown' sputum described by the patient could be a sign of an infective process, but it could also be haemoptysis (which is typical of PE).
The chest X-ray demonstrates several hallmark signs of PE: a prominent right pulmonary artery (Fleischner sign), abrupt cut-off of the vessel (Knuckle sign), and peripheral oligaemia in the right lung. These findings indicate a large embolus obstructing the right pulmonary artery, leading to reduced perfusion in the affected lung region and increased pressure proximally.
This ECG demonstrates several findings consistent with PE:
Sinus tachycardia
S1Q3T3
RBBB
Diffuse (including inferior) repolarisation abnormalities, such as T-wave inversion and ST depression
On ECG, the most common finding in acute PE is sinus tachycardia. This reflects the body's response to hypoxaemia and increased sympathetic drive due to impaired pulmonary circulation. Sinus tachycardia is defined by a regular rhythm with a rate above 100 bpm, normal P waves preceding each QRS complex, and a consistent PR interval. It is a non-specific but highly prevalent finding in PE, seen in the majority of cases, especially in the acute setting.1
Other ECG changes that may be seen in PE include right heart strain patterns such as right bundle branch block, T-wave inversion in the right precordial leads (V1–V4), and the classic but rare S1Q3T3 pattern (deep S wave in lead I, pathological Q wave in lead III and T-wave inversion in lead III). However, these are much less common than sinus tachycardia. Pathological Q waves in inferior leads are more typical of myocardial infarction, and atrial arrhythmias are not the predominant finding in PE.
Summary
This case highlights the importance of maintaining a high index of suspicion for pulmonary embolism (PE) in patients presenting with chest pain, especially when accompanied by hypoxia, tachycardia, and non-specific systemic symptoms like fever and cough.
The ECG, though often non-specific, can reveal valuable clues—most commonly sinus tachycardia, along with patterns of right heart strain such as S1Q3T3 and T-wave inversions. Similarly, chest X-ray findings like the Fleischner and Knuckle signs, and peripheral oligaemia, can support the diagnosis when interpreted in context.