What you’ll learn from this post
After reading this post, you will learn about the multifocal atrial rhythm (also known as wandering atrial pacemaker) and multifocal atrial tachycardia (MAT).
You will learn:
Their ECG features
Why they look like atrial fibrillation (AF)
Why they are important to know
What you need to do once you’ve seen them (without unnecessary details)
Multifocal Atrial Rhythm
What is a multifocal atrial rhythm?
As the name implies, it’s a rhythm where you don’t have a single focus firing in the atria but multiple foci. Sinus rhythm has a single focus: the sinoatrial (SA) node. Focal atrial rhythms also have a single focus: it’s just not the SA node.
The multifocal atrial rhythm has many atrial foci firing! This rhythm is also termed Wandering Atrial Pacemaker.
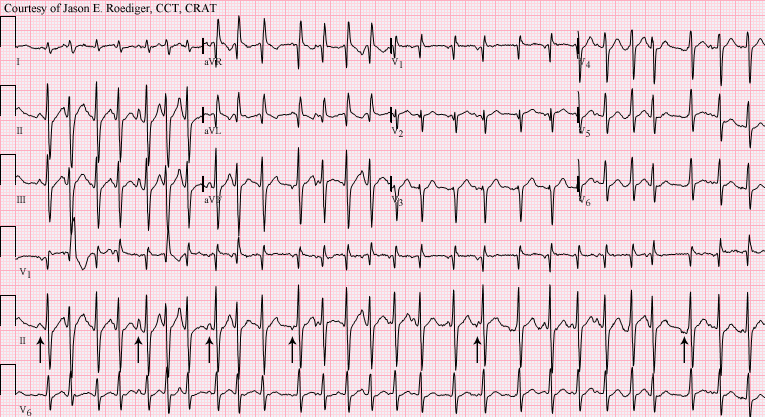
The ECG features of multifocal atrial rhythm
≥ 3 P wave morphologies (as there are ≥ 3 ectopic foci firing) - with variable PR intervals
The rhythm is irregularly irregular (similar to AF)
The atrial rate is normal (60-100 bpm) [1]

Variable PR intervals: The PR interval changes as every P wave has its own PR interval because different foci have different distances from the AV node.
Irregularly irregular: Every atrial focus has its own pacing settings. Focus A might be firing 70 times per minute, whereas focus B is firing 90 times per minute. Therefore, you end up with variable P-P intervals (they are not the same because the P waves come from different foci with different settings). This is how you get an irregularly irregular rhythm. [1]
This is why you might think it’s atrial fibrillation (AF). Contrary to AF, you can still clearly see P waves in multifocal atrial rhythm. In AF, you might see atrial activity or not:
Coarse AF: You can see the fibrillatory waves (known as “f waves”)
Fine AF: Atrial activity might be very difficult to distinguish based on a transthoracic ECG.
It’s like seeing too many premature atrial ectopics on a single rhythm strip.1
Multifocal Atrial Tachycardia (MAT)
Multifocal atrial tachycardia (MAT) is similar to a multifocal atrial rhythm (or wandering atrial pacemaker) in that there are three or more independent atrial ectopic foci, except that the heart rate is greater than 100 bpm. [1]
MAT is an uncommon but not rare arrhythmia. It has been estimated to occur in 0.37% of hospitalised patients. [2]
Why should you know about MAT?
The main reason why MAT is important is underlying pathology.
It is thought that MAT is caused by right atrial abnormality (hypertension and distension). [2]
So, when you see MAT, think about the causes of right atrial abnormality.
What are the causes of right atrial abnormality?
Pulmonary hypertension
Left ventricular dysfunction
These are the two most important ones. Why?
Taking a quick glance at the anatomy will help you understand it better.

Look at the right atrium. What structures are downstream of the right atrium?2
A big part of cardiology (and medicine in general) is understanding this:
Obstructions in blood circulation can damage the body by increasing pressure before the obstruction and reducing supply after.
And when I say obstruction, it can be anything that raises the hydrostatic pressure.
Let’s say you have chronic severe COPD. This can lead to pulmonary hypertension. [3] Then, pulmonary hypertension will strain the RV and, subsequently the RA. Therefore, you can get RA distension (appearing as P pulmonale on the ECG), which can cause MAT.
Similarly, you can get RV impairment from LV impairment. In fact, the most common cause of RV failure is LV failure. [4] LV failure leads to increased pressures in the structures preceding the LV, like the LA (causing LA enlargement, presenting as P mitrale on the ECG), the pulmonary vasculature (causing pulmonary hypertension; fluid leaks inside the alveoli due to raised pressures and you get pulmonary oedema) etc.
Therefore, pulmonary hypertension and LV failure are the most important things you should consider when seeing MAT.
Other clinical conditions associated with MAT
Apart from respiratory and cardiac causes, when you see MAT, consider the following:
Hypokalaemia
Hypomagnesaemia
Drugs (can induce or exacerbate MAT, especially in the presence of respiratory disease)
Isoproterenol
Aminophylline
Theophylline
Chronic renal failure
Sepsis
Recent surgery (especially if associated with respiratory or cardiac failure) [2]
Management principles
Step 1: Manage the underlying cause
As you might have thought already, the first and most important step is to identify and manage the underlying pathology, which most likely is going to be a respiratory or cardiac problem.
Step 2: Correct electrolyte abnormalities
After that, before you even consider rate control and all that fancy stuff, check the electrolytes, specifically potassium and magnesium. Replace them if they are low.
Step 3: Control the rate directly if needed
Lastly, and most likely not something that most of us will need to do, is rate control IF the rhythm causes sustained rapid ventricular response, which causes or worsens myocardial ischaemia, heart failure, syncope or shock.
Contrary to AF, digoxin doesn't play an important role here; rate control is primarily achieved with:
non-dihydropyridine calcium channel blockers (i.e. verapamil or diltiazem)
beta-blockers
But I would get senior advice here (in step 3) if I were you (unless you’re more senior than me, in which case do as you think it’s appropriate 😅).
Conclusion
So this is MAT, the rhythm that most ECG interpreters will see and say: “Oh, atrial fibrillation!”. But you won’t make that mistake!
MAT is uncommon - it occurs in around 0.37% of hospitalised patients
MAT and AF are the two rhythms that are, typically, irregularly irregular
The reason MAT is important to know is because it raises the suspicion of an underlying disease, especially from the cardiopulmonary system
References
Jordan M. Prutkin. ECG tutorial: Atrial and atrioventricular nodal (supraventricular) arrhythmias. Post TW, ed. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2022.
Alfred Buxton. Multifocal atrial tachycardia. Post TW, ed. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2022.
Zakynthinos E, Daniil Z, Papanikolaou J, Makris D. Pulmonary hypertension in COPD: pathophysiology and therapeutic targets. Curr Drug Targets. 2011 Apr;12(4):501-13. doi: 10.2174/138945011794751483. PMID: 21194405.
Mandras SA, Desai S. Right Heart Failure. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459381/
To refresh your memory about premature complexes, read the following two posts:
RA: right atrium, RV: right ventricle, PulmCirculation: pulmonary circulation (vasculature), LA: left atrium, LV: left ventricle, SystemCirculation: systemic circulation (vasculature)